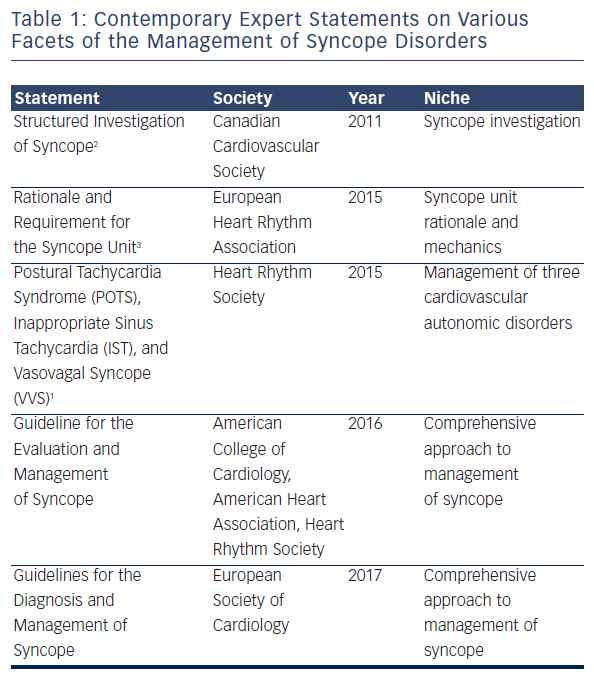
Syncope and palpitations are two common clinical presentations, and both pose difficulties in the approach to their management. They are both symptoms of a number of syndromes, and an efficient approach with targeted therapy is challenging. Cardiac arrhythmia specialists, who lack a compact and accessible guide to management, see many patients with these symptoms in consultation. Recognising this, in 2015 the Heart Rhythm Society (HRS) released an expert consensus document1 on three common syndromes: postural tachycardia syndrome (POTS), inappropriate sinus tachycardia (IST), and vasovagal syncope (VVS). This focused statement is complemented by several other contemporary reports (see Table 1): the 2011 Position Statement on Structured Investigation of Syncope by the Canadian Cardiovascular Society,2 the 2015 Position Statement for the Rationale and Requirement for the Syncope Unit3 by the European Heart Rhythm Association (EHRA), the 2016 Guideline for the Evaluation and Management of Syncope being prepared by the American College of Cardiology (ACC), the American Heart Association (AHA) and the HRS. The 2017 Guidelines for the Diagnosis and Management of Syncope are being prepared by the European Society of Cardiology (ESC).
The consensus recommendations in this document use the class I, IIa, IIb and III classifications and the corresponding language used by the ACC at the time of the expert consensus document’s publication.1 Class I is a strong recommendation, denoting benefit greatly exceeding risk. Class IIa is a somewhat weaker recommendation, denoting benefit probably exceeding risk, and class IIb denotes benefit equivalent to, or possibly exceeding risk. Class III is a recommendation against a specific treatment because either there is a lack of benefit or there is harm. Level A denotes the highest level of evidence, usually from multiple clinical trials with or without registries. Level B evidence is of a moderate level, either from randomised trials (B-R) or well-executed non-randomised trials (B-NR). Level C evidence is from weaker studies with significant limitations and level E is simply a consensus expert opinion in the absence of credible published evidence.
Here we will review contemporary, expert advice on the management of POTS, IST and VVS. We will highlight important issues and clarify and expand on several key points from the HRS expert consensus document.
Definitions
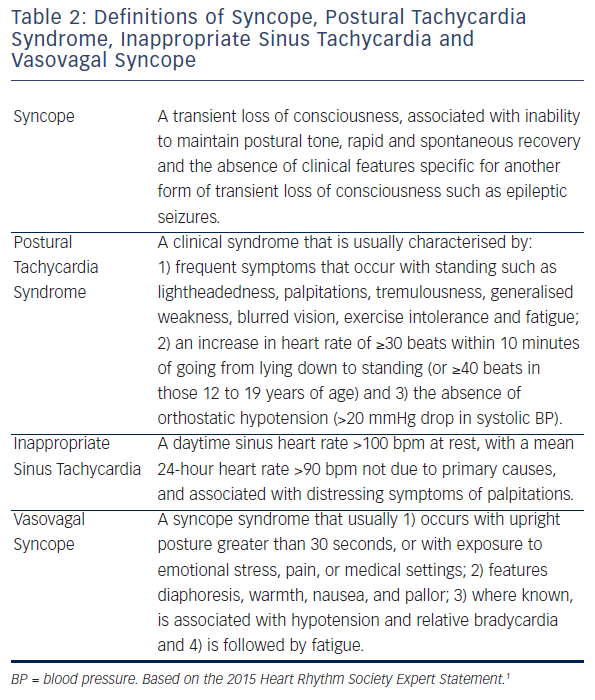
The HRS writing group recognised the importance of providing simple, clear definitions that could be used at the bedside and uniform criteria for inclusion of subjects into studies (see Table 2).
Definition of Syncope
Originally syncope was defined as a transient state of unconsciousness characterised by spontaneous recovery or recovery in the supine position.4 This definition was developed to describe tilt test outcomes and was not sufficiently descriptive for clinical use. Subsequently, the ESC defined syncope as a transient episode of loss of consciousness that is due to transient global cerebral hypoperfusion characterised by rapid onset, short duration and spontaneous complete recovery.5 This definition was more specific and included a pathophysiological basis for syncope. Unfortunately, the criterion of ‘global cerebral hypoperfusion’ proved challenging for clinicians dealing with transient loss of consciousness in clinical practice. In September 2013 a multi-specialty workshop of North American and European syncope experts met in Gargnano, Italy. At that consensus conference,6 the physiological criterion for syncope was removed, and a criterion that excluded other causes of loss of consciousness was substituted. This practical approach met with agreement by cardiologists, neurologists, internists, family doctors and emergency department physicians. The HRS document1 minimally modified the Gargnano definition of syncope (see Table 2).
Definition of Postural Tachycardia Syndrome
The HRS definition of POTS (see Table 2) is based on the criteria outlined by the American Autonomic Society7. POTS is a syndrome that may actually be a collection of several disorders. POTS is also systemic and chronic and should persist for at least 3–6 months prior to diagnosis. Patients are not only troubled by postural tachycardia, but usually have other symptoms including tremulousness, generalised weakness, blurred vision, exercise intolerance, perceived inability to think clearly and fatigue. Significant orthostatic hypotension precludes the diagnosis of POTS. Postural tachycardia must develop within 10 minutes since prolonged head-up tilt causes excessive tachycardia in many healthy subjects.
Definition of Inappropriate Sinus Tachycardia
IST is a clinical syndrome and not just a physiological manifestation, so the definition of IST is based on both symptoms and heart rate criteria (see Table 2).1 IST, as a clinical syndrome, requires the element of distress. Not everyone with sinus tachycardia is distressed by their tachycardia and therefore do not have IST. The specific heart rate criteria are based on the distributions of normal heart rates and are only modestly specific and sensitive. A good deal of clinical judgment is required in establishing the diagnosis.
Definition of Vasovagal Syncope
The HRS document defines VVS as a syncope syndrome that usually 1) occurs with upright posture greater than 30 seconds, or with exposure to emotional stress, pain or medical settings; 2) features diaphoresis, warmth, nausea and pallor; 3) where known, is associated with hypotension and relative bradycardia, and 4) is followed by fatigue1 (see Table 2). The definition of VVS is based on published reports of symptoms of patients with positive tilt tests compared with those known or believed to have other disorders.8–12 The >30 second time requirement is intended to exclude patients with initial orthostatic hypotension.
Postural Tachycardia Syndrome
Presentation
POTS occurs in about 0.2 %7,13,14 and usually presents in young women between the ages of 15 and 45 years.13–18 It is a systemic illness whose main symptoms are orthostatic: lightheadedness, palpitations and tremulousness; gastrointestinal: bloating, nausea, diarrhoea, abdominal pain; and systemic: exercise intolerance, fatigue, sleep disturbance and migraine headaches.15 The symptoms of POTS are commonly exacerbated by dehydration, heat, alcohol and exercise. Many patients with POTS faint occasionally, although presyncopal episodes are much more common.
There are few data about the long-term outcome. POTS is chronic, without known mortality, and many patients seem to improve over time. POTS has documented abnormalities in several pathophysiological processes19 including autonomic denervation, hypovolaemia, hyperadrenergic stimulation, deconditioning and hypervigilance. Multiple mechanisms may co-exist in some patients.
Diagnosis
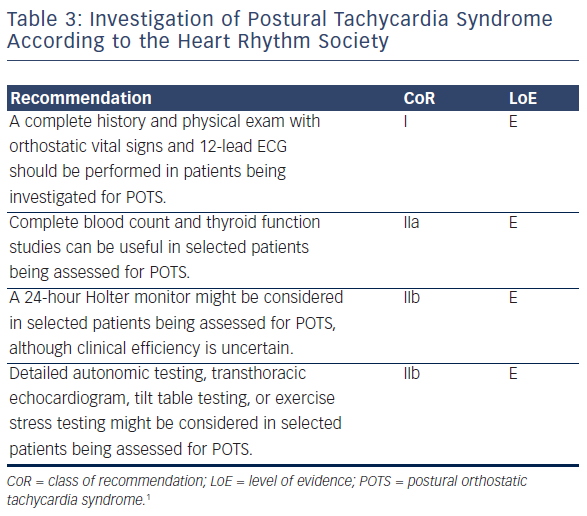
Patient suspected of having POTS should receive a complete history and physical examination with orthostatic vital signs and a 12-lead ECG (see Table 3). The history should define the chronicity of the condition, potential causes of orthostatic tachycardia, modifying factors, impact on daily activities and family history (see Table 3). A dietary history of salt and water intake is valuable and an autonomic system review should assess for symptoms of an autonomic neuropathy. The increase in heart rate with standing decreases slowly with advancing age20 and the standing heart rate may be ≥120 bpm in severe forms.7,16 Slightly higher values occur in the morning.21 If orthostatic vital signs in the clinic are nondiagnostic and the clinical suspicion for POTS is high, a tilt table test can be helpful.
A 24-hour Holter monitor can document that the tachycardia is indeed sinus tachycardia. A thyroid function test (for hyperthyroidism) and haematocrit (for anaemia) and transthoracic echocardiogram (to exclude a cardiomyopathy) can be useful in selected cases but should not be performed routinely. If the patient’s symptoms do not markedly improve then formal autonomic function testing should be considered.
Treatment
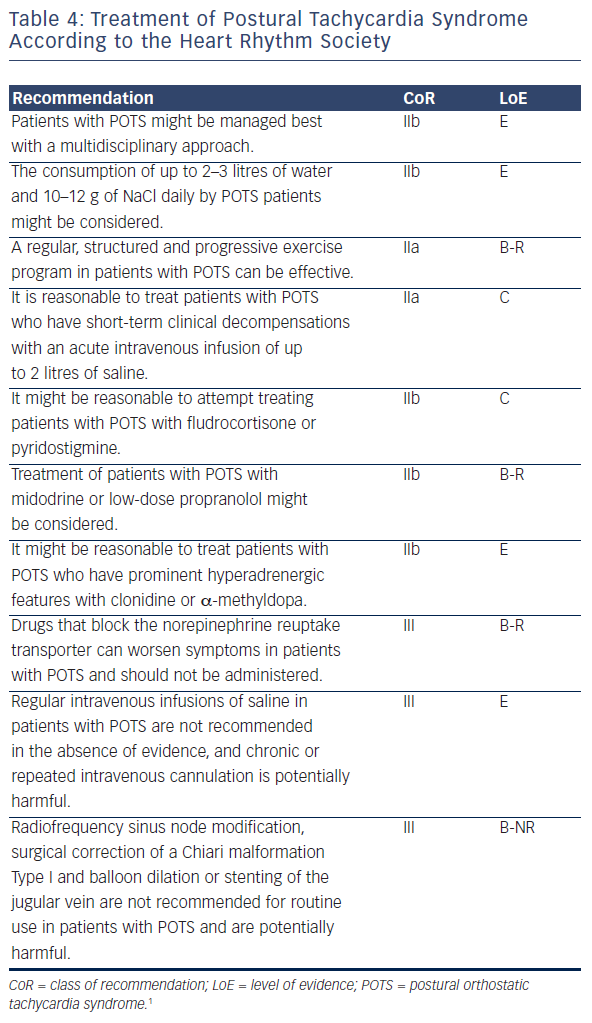
There are no therapies that are uniformly successful, and combinations of approaches are often needed (see Table 4). Few treatments have been tested with the usual rigour of randomised clinical trials and there is a lack of a consensus as to whether specific treatments should be targeted to subsets of POTS, or whether a uniform approach to all should be used.
Treatment might be provided more comprehensively with collaborative approaches by multiple disciplines including physicians, psychologists, nurses, physical therapists, occupational therapists and recreational therapists (see Table 4).22 Conservative treatments should be tried first in all patients. These include withdrawing medications that might worsen POTS, use of compression garments and limiting gravitational deconditioning. Patients should engage in a regular, structured, graduated, supervised exercise program featuring aerobic reconditioning with some resistance training of the thighs,23,24 starting with non-upright exercises. Exercise programs can be effective even outside of formal exercise training centres.22 Patients with suspected hypovolaemia should drink at least 2–3 litres of water per day and dietary salt intake should be about 10–12 g/day if tolerated, including salt tablets if necessary.25
Fludrocortisone might be useful in the treatment of POTS through enhanced sodium retention and plasma volume expansion, although its effectiveness for POTS has not been tested in randomised clinical trials.26 Its biological effects can take about one week to reach a steady state. Midodrine is a prodrug whose metabolite is a peripheral alpha-1 adrenergic receptor agonist that constricts both veins and arteries. It significantly reduces orthostatic tachycardia.27 Midodrine has a rapid onset and short half-life, requiring dosing up to 3 times daily during daytime hours. It should not be taken within 4–5 hours of bedtime, as it may cause or worsen supine hypertension.
Low-dose oral propranolol (10–20 mg) is effective at lowering standing heart rate and may improve symptoms in POTS patients acutely, while higher doses are less effective.28 Long-acting propranolol does not improve quality of life (QoL) in POTS patients.29 Other β-blockers have not been studied. Ivabradine slows sinus rates without impacting blood pressure. About 60 % of POTS patients treated with ivabradine in an open-label study improved.30 However ivabradine is not widely available.
Pyridostigmine is a peripheral acetylcholinesterase inhibitor that increases synaptic acetylcholine in the autonomic ganglia and at peripheral muscarinic receptors. It blunts orthostatic tachycardia31 and may improve chronic symptoms in most patients,32 but has side-effects including diarrhoea and abdominal pain that can limit its tolerability.
Central sympatholytic agents can be useful in patients with very hyperadrenergic features such as orthostatic hypertension with excessive tachycardia (hyperadrenergic POTS), but may not be as well tolerated in neuropathic POTS where a peripheral neuropathy might compromise venous return from the lower extremities. Clonidine can blunt tachycardia and hypertension in patients with hyperadrenergic POTS,33 although methyldopa with its longer half-life is sometimes better tolerated.34 Both drugs can cause drowsiness, fatigue and worsen mental clouding. Modafinil might help the fatigue and cognitive dysfunction seen in some patients35 with only a minimal increase in tachycardia.36
Radiofrequency sinus node modification for the sinus tachycardia of POTS is not recommended as this often worsens symptoms and occasionally makes the patient pacemaker dependent.37 Some centres decompress the cerebellar tonsils38 or perform jugular venoplasty39 in an effort to ‘cure’ POTS. These are potentially dangerous and costly procedures without credible evidence of effectiveness in the treatment of POTS. They should not be offered to patients until prospective controlled data demonstrate its efficacy.
Syndrome Of Inappropriate Sinus Tachycardia
Presentation
The prevalence of the heart rate criteria for IST was estimated in a middle-aged population of men and women to be 1.2 %.40 This includes both symptomatic and asymptomatic subjects. There is a general sense that IST is chronic with no known mortality, but whether and how quickly patients improve is unknown. The pathophysiology is incompletely understood. It is likely that there are several different underlying pathologies that can result in this syndrome, including increased sinus node automaticity,41 increased sympathetic activity42 and sensitivity, decreased parasympathetic activity41 and impaired neurohumoral modulation.
Diagnosis
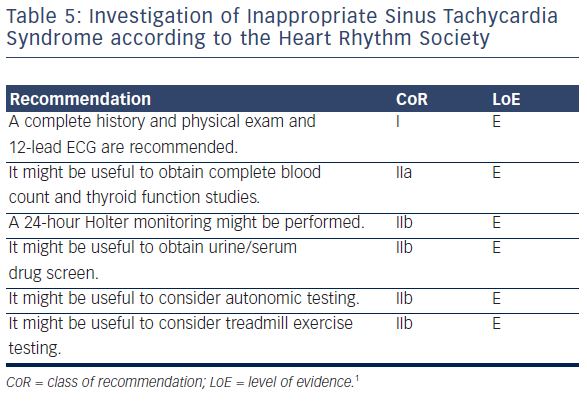
A thorough history and physical exam should be performed focusing on possible causes of sinus tachycardia such as volume depletion, thyroid disease, drug use, psychological triggers, panic attacks and POTS (see Table 5). A 12-lead ECG is useful in documenting tachycardia and in demonstrating sinus rhythm. A 24-hour Holter monitor can be useful in confirming the diagnosis, since one of the criteria is based on average 24-hour heart rate. Treadmill exercise testing might be useful to document an exaggerated tachycardia response to exertion.42 Cardiovascular autonomic testing is rarely useful.
Treatment
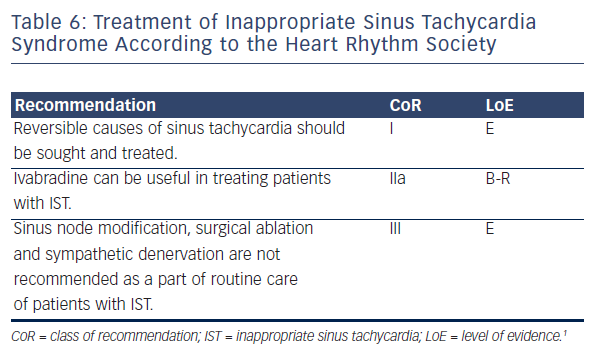
There are no positive long-term prospective clinical trials of any therapeutic intervention and symptoms may continue despite heart rate control. IST patients nearly always present distressed about the complexity of their problems. Lifestyle changes should be discussed early with all patients. β-adrenergic blockers may cause side-effects and should be used judiciously (see Table 6). Ivabradine holds considerable promise for the treatment of IST. It blocks the If current, is generally well tolerated and has a remarkable effect on heart rate. At doses of 5–7.5 mg twice daily it slows heart rate by 25–40 bpm.43,44 Ivabradine is not available in all countries but is likely to become increasingly so in the next 2–3 years.
Several groups have reported on the modification or ablation of the sinus node in IST. Primary success rates are usually good, but the complication rates are significant. These include requirement for permanent pacing, transient or permanent phrenic nerve paralysis and transient superior vena cava syndrome. There is no evidence for long-term symptomatic improvement with radiofrequency ablation for IST. Patients and physicians alike need to be aware that while patients may be highly motivated, the consequences of aggressive therapeutic attempts can seriously outweigh any potential benefit.
Vasovagal Syncope
Presentation
VVS is very common. By age 60, 42 % of women and 32 % of men will have had at least one vasovagal faint,45,46 and most patients faint recurrently. VVS is manifested in about 1–3 % of toddlers as syncope with reflex anoxia or breath holding, and the incidence begins to increase markedly around age 11 years. The median age of first faint is about 14 years and most people with VVS have had their first faint before age 40 years.47 In specialist syncope clinics, late first presentations do occur with some regularity. The outcome of VVS patients is generally benign in that there is no increased mortality, but there is a high rate of recurrence. The overall 1-year recurrence rate in many reports is about 25–35 %.48 Those patients with recurrent VVS often have a significant loss of QoL.49 Fortunately most patients improve in the absence of specific therapy after assessment.50
Diagnosis
The most important step in the diagnosis of VVS is an excellent and evidence-informed history. The key diagnostic features are in four categories: predisposing situations, prodromal symptoms, physical signs and recovery time and symptoms. VVS usually occurs after prolonged standing or in a sitting position, but can be triggered even in the supine position by exposure to medical or dental situations, pain, or scenes of injury. Prolonged can mean as little as 2–3 minutes and this is a key feature distinguishing VVS from initial orthostatic hypotension, in which syncope occurs within the first few seconds of standing up. Prodromal features include progressive presyncope, diaphoresis, a sense of warmth or flushing, nausea or abdominal discomfort and visual blurring or frank loss of vision. While unconscious the patient is usually still, but both fine and coarse myoclonic movements are witnessed about 10 % of the time and can lead to diagnostic confusion with epilepsy.51 Unconsciousness usually lasts less than 1–2 minutes, but full recovery can be sluggish. Patients are usually very tired for minutes to hours following a syncopal spell. Further investigation usually is not needed.52 Diagnostic scores have been developed based on subjects with rigorously defined diagnoses.12,53,54 Generally, attempts at validation have not been done with subjects as rigorously defined.55,56 Although the scores report overall high degrees of accuracy, they may need revision and validation in larger populations. Nonetheless, they serve as useful reminders of important diagnostic points, and form reproducible criteria for entry into observational, genetic and randomised controlled interventional trials.
Tilt Table Testing
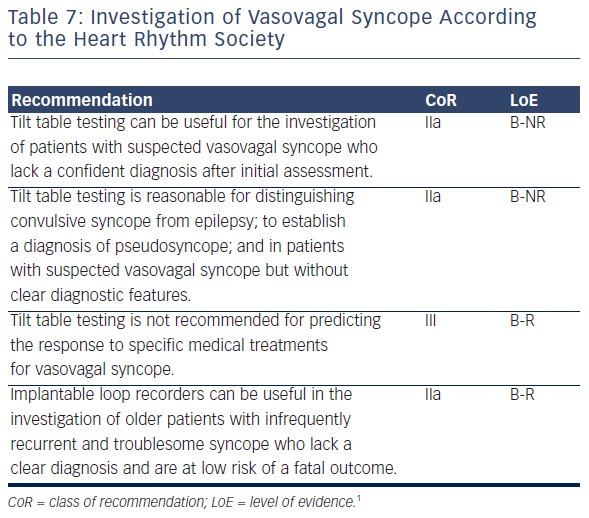
The usefulness of investigation strategies depends on the patient mix and the purpose of the investigation (see Table 7). In most cardiology settings it is most important to determine whether patients have arrhythmic causes of syncope. Generally there are two approaches to discern arrhythmic syncope: determining whether the patient has the substrate for particular kinds of syncope and determining directly whether patients have syncope associated with specific heart rhythm abnormalities or characteristics.
Another important differential diagnosis for VVS is neurogenic orthostatic hypotension, which is often caused by autonomic nervous system failure. Blood pressure usually falls reproducibly and rapidly within three minutes of upright posture. Unlike VVS which has an intermittent reflex with a relative drop in heart rate and hypotension, autonomic failure is often associated with a fixed heart rate a persistent failure of vasoconstriction.57 Formal autonomic testing including a Valsalva manoeuvre can demonstrate this failure of vasoconstriction. Orthostatic hypotension was not explicitly discussed in the HRS expert consensus document.
Head-up tilt table tests (see Table 7) feature prolonged passive postural stress to determine whether patients have the autonomic substrate for VVS. In cardiology clinics, this is often accompanied by triggering agents such as isoproterenol, nitrates or clomipramine. However, with increasingly aggressive protocols comes increased sensitivity, but also the likelihood of decreased specificity. The tilt test may prove useful in elderly patients due to the difficulties in obtaining an informative history in some older patients and due to its usefulness in identifying the cause of unexplained falls.58
There are specific circumstances in which tilt table testing can be helpful (see Table 7). It can help distinguish convulsive syncope from true seizure activity; help in situations where, despite careful questioning, the cause of syncope remains unclear and establish a diagnosis of pseudosyncope. The latter is a poorly understood syndrome of apparent syncopal episodes in the absence of haemodynamic changes that might cause cerebral hypoperfusion.
There are several current knowledge gaps regarding the use of tilt table testing. First, the tilt test has not been validated prospectively against populations with rigorously defined VVS. Second, there is no ‘ideal’ protocol, in that there is an inexorable trade-off between sensitivity and specificity. Also, the supplemental role of tilt testing when added to histories taken by experts, with or without quantitative diagnostic scores, has not been assessed. The indications for tilt testing are a matter of expert consensus.59
Prolonged Electrocardiographic Monitoring
The current gold standard for diagnosing syncope due to cardiac arrhythmias is recording an ECG during an episode of clinical syncope (see Table 7). The diagnostic yield increases with the duration of monitoring and is significantly higher with implanted monitors. External monitors have a loop memory that continuously records and overwrites the ECG until activation records an ECG strip. Diagnostic sensitivity is at best 10–25 % after one month of monitoring. Implanted loop recorders are subcutaneous devices that last up to three years, storing the ECG retrospectively when activated by the patient after a syncopal episode, and also after automatic detection based on rate or rhythm criteria.
Implantable loop recorders (ILR) deliver a diagnosis in about 35 % of patients. Importantly, there have been randomised controlled trials of their clinical effectiveness, and the results consistently show that in older patients with unexplained syncope these devices should be used early rather than later in investigation.59–62 However, they have only been shown to improve care in the subset of patients who are older, have asystole documented on the ILR and a negative tilt test. These patients may benefit from permanent pacing.63,64
Conservative and Medical Treatment for Vasovagal Syncope
VVS is generally benign and seems to feature clusters of syncope interspersed with long quiescent periods. Older and younger individuals differ markedly, with complicating comorbidities and medical therapies more common in older patients. Despite its usually apparently benign profile, some patients with frequent episodes of VVS require active treatment. It is important to balance natural history, the potential for harm and the marked reduction in syncope seen in all control arms of randomised trials with symptom severity and the overall likelihood of treatment effectiveness.
Education, reassurance and encouraging salt and fluid intake are indicated in patients with VVS where not contraindicated. Reducing medications that cause hypotension might be helpful, provided that it is feasible (see Table 8). Increasing salt and fluid intake may be helpful where it is safe. In general, long-term placebo-controlled prospective trials have not been encouraging.
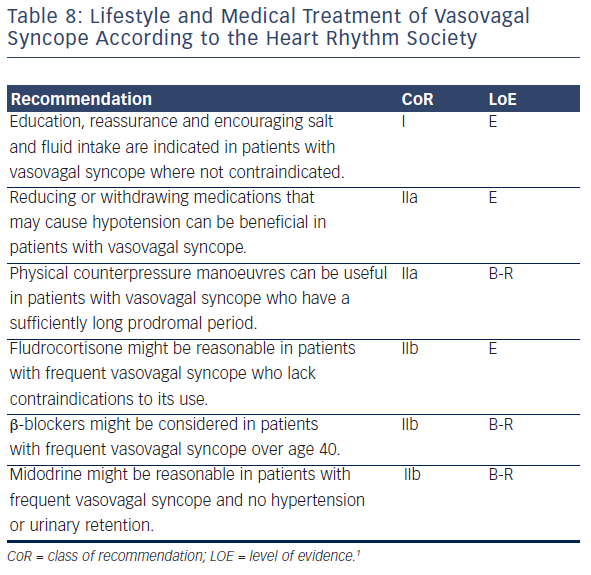
Physical Counter Pressure Manoeuvres
Isometric exercise of large muscles causes a blood pressure increase during the phase of impending reflex syncope on tilt tests, preventing or delaying loss of consciousness. Physical counter pressure manoeuvre reduced the likelihood of fainting by 39 % in one randomised prospective clinical trial.65 However, syncope recurred in a substantial minority of patients, and the study was open label. Nonetheless, physical counterpressure manoeuvres are largely free of risk and should constitute a core of management of patients with VVS of all severities.
β-blockers
These drugs have not been found to be effective in adequately designed and controlled randomised studies. The largest prospective, placebo-controlled, randomised critical trial of β-blocker therapy was the Prevention of Syncope Trial (POST) in which metoprolol was compared with placebo in patients with tilt-positive presumed VVS.66 While the overall result was negative, there was evidence of benefit in patients >40 years in a meta-analysis of a prespecified and prestratified substudy of POST and a large earlier observational study.67 In the absence of compelling evidence, it is not unreasonable to attempt therapy with metoprolol in older patients and to avoid using it in younger patients.
Fludrocortisone
The POST2 randomised clinical trial comparing fludrocortisone with placebo for VVS was recently completed.68 There was a strong trend to a significant benefit from fludrocortisone (p=0.07). In the absence of more compelling evidence, the HRS authors felt it might be reasonable to attempt therapy with fludrocortisone in patients whose symptom severity merits it.
Midodrine
Five randomised trials of midodrine showed a consistent risk reduction of about 70 %.69 However, due to selection or design issues, none provide high-level evidence for adults. The major limitations of midodrine are frequent dosing, effects on supine hypertension, and lack of knowledge of its teratogenic effects. Older males may develop urinary retention. In the absence of compelling evidence, it might be reasonable to attempt therapy with midodrine in patients whose symptom severity merits it.
Selective Serotonin Reuptake Inhibitors
Based on a solid biological rationale, there have been several observational studies and three small randomised trials of serotonin transport inhibitors for the prevention of VVS.70–72 Results have been mixed and there remains considerable uncertainty about the effectiveness these drugs in preventing syncope.
Treatment Strategy
For patients with only an occasional faint, the physician should reassure, advocate increased fluid and salt intake and teach counterpressure manoeuvres. Patients who have not fainted in the previous year should not receive attempts at medical therapy. For patients with recurrent episodes, begin conservatively and attempt to reduce drugs that might cause hypotension. For patients with recent recurrent episodes of VVS, it is reasonable to consider fludrocortisone, midodrine or β-blockers (if older than 40 years) prior to pacing, recognising that there is no high-level evidence for their use.
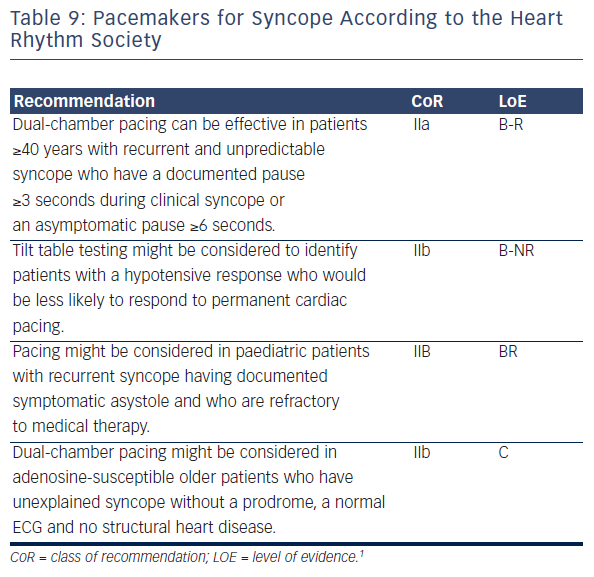
Pacemaker Treatment
Cardiac pacing has a very limited role in patients with typical VVS (see Table 9). There are no positive, placebo-controlled studies of pacemakers in patients with VVS under age 40 years, and in these patients cardiac pacing should be the last choice. Pacing should be considered only in highly selected patients, i.e. those well over 40 years of age, affected by frequent recurrences associated with frequent injury, limited prodrome and documented asystole. Prolonged ECG monitoring, usually by an implantable loop recorder, is often necessary.63,64 There is emerging evidence that tilt table testing identifies patients with predominant reflex hypotension.63,64 Accordingly, tilt table testing may be performed to assess hypotensive susceptibility and identify patients who may not respond to permanent cardiac pacing. Although the documentation of a prolonged asystolic reflex during tilt table testing predicts a similar response during spontaneous syncope, the benefit of pacing in positive cardioinhibitory tilt patients remains uncertain.63,64
Conclusions
VVS, POTS and IST are all clinical syndromes that are poorly understood by physicians, associated with significant morbidity (but not mortality) for the patients, and significant frustrations for both patients and their physicians. The 2015 Heart Rhythm Society Expert Consensus Statement on the Diagnosis and Treatment of Postural Tachycardia Syndrome, Inappropriate Sinus Tachycardia, and Vasovagal Syncope provides physicians with an introduction to these disorders and initial recommendations on their investigation and treatment. This statement should not be read as an all-inclusive ‘Bible’, but rather as a practical working document. Optimal care for our patients is likely to require going beyond this statement to personalise care to the individual.